
Former offensive lineman Jamaal Jackson once said, "Your first day in the league is the last day you'll ever be 100% healthy." No muscle, ligament, joint, tendon or organ is safe. Sooner or later, every NFL player will end up in the training room and on the weekly injury report.
Whether you're a fantasy football enthusiast or a fan worried about your favorite team's star player, you'll want to have a basic understanding of football related injuries, their treatments and expected recovery times. In this primer, you'll find information about how the most common and severe football injuries occur, how they're treated and how soon you can expect a player to recover and return to play. We'll also discuss the new orthobiologic treatments that are gaining popularity (e.g. platelet-rich plasma, stem cell therapies, etc) and some of the more common pain-killing injections players receive during the week.
Muscle Strains
Strain vs Sprain
Though commonly used terms, strain and sprain are often used confusingly or interchangeably in the media. While seemingly small distinctions, it's important to define the differences in terms and clarify one important common misconception about them.
A strain is an injury to a muscle or tendon. A sprain is an injury to a ligament. Players strain their hamstring muscle or Achilles tendon and sprain the ligaments in their knee, ankle, or shoulder. By definition, a strain or sprain is a tear of the fibers of the muscle, tendon or ligament, even injuries of the mildest grade.
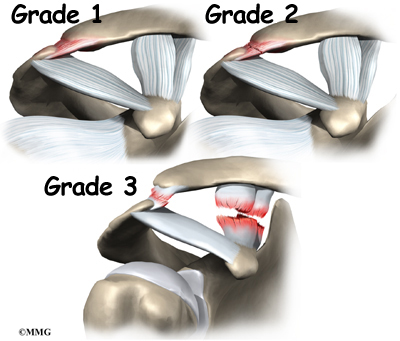
There are three grades of strains or sprains. A Grade 1 injury involves stretching and micro-tearing of tissue fibers. They're commonly referred to as muscle pulls or mild ligament strains. Grade 2 injuries encompass a wide range of partial tearing of tissue fibers, from just a small percentage of the structure to a large percentage and are usually accompanied by swelling and bleeding within the structure itself. Grade 3 injuries are complete tears or ruptures of the muscle, tendon or ligament. A torn ACL, ruptured hamstring, bicep or pectoral muscle and torn Achilles tendon are all examples of Grade 3 injuries.
Hamstring/Quadricep/Calf Muscle Strain
Muscle strains are among the most common football injuries. Frustratingly, they're also associated with unclear recovery timetables and the risk of recurrent and more severe injuries when players return to play before they're 100% recovered.
There is no standard return to play expectation after a muscle strain. The percentage of muscle fibers torn, proximity of the tear to the tendon, amount of bleeding within the muscle belly and the rapidity at which a player usually heals all factor into the vague timetables reported by the player and his team. While we often hear that players with Grade 1 muscle strains are expected to recover in zero to two weeks, Grade 2 strains two to six weeks and Grade 3 strains four to eight weeks or longer, teams re-evaluate these injuries on a week-to-week basis.
Players are considered safe to return to football-related activity when they can function without pain or tightness and the injured muscle is around 90-95% as strong as the healthy muscle on the other side. Still, players are at high risk of re-injury in the first few days after returning and a recurrence of the muscle strain is often more severe than the initial injury. Cascade injuries - an injury that occurs when an athlete has unconsciously stressed another part of his body to compensate for a previous injury - are another potential consequence of an early return to play. In general, you should be wary of a player who returns at the most optimistic end of his recovery timetable.
Shoulder Injuries
Acromioclavicular (AC) joint sprain (Shoulder Separation)

The AC joint is a joint at the top of the shoulder where part of the shoulder blade (the acromion of the scapula) and the collarbone (clavicle) meet. Like the knee, ankle and elbow, there are a number of ligaments that hold the joint together. An AC joint sprain, or shoulder separation, occurs when one or more of these ligaments are stretched or torn, which most often happens when a player is driven into the turf shoulder first.
As with any sprain, there are grades of severity of AC joint injuries. Grade 1 injuries are relatively minor and involve mild stretching and microtears of the ligament fibers. Grade 1 injuries are usually treated with ice, sling immobilization and anti-inflammatories and players are at low risk of missing snaps the following week.
Grade 2 and 3 injuries are more severe, with increasing amounts of damage to the ligaments stabilizing the joint. In a Grade 3 injury, all ligaments are completely torn and the collarbone is no longer tethered to the shoulder blade. Most Grade 2 injuries are treated with ice, rest/rehab and sling immobilization, with return to play within one to four weeks (depending on the severity of the sprain). Grade 3 injuries can be treated without an operation, but many NFL players choose surgical treatment to limit the risk of chronic pain and range of motion problems. Recovery time following AC joint surgery is often four to six months.
Shoulder Subluxation/Dislocation
Though sometimes confused with shoulder separations, partial (subluxation) and complete dislocations of the shoulder occur at a different part of the joint. The most common type of shoulder dislocation occurs when the arm is extended away from the body and pulled backward, with the upper arm bone (humerus) pulled forward and out of the shoulder socket.
During the dislocation, the cartilage, ligaments, and muscles around the shoulder joint can be damaged, leading to varying degrees of instability in the joint. The presence and degree of these labral cartilage tears, fractures to the upper arm bone, and ligament tears determine the likelihood of future dislocations and whether surgery may be recommended. Players may choose to play through minor injuries with the aid of pain relievers and a harness. If surgery is necessary, recovery and rehabilitation usually take four to six months.
Clavicle Fracture
The clavicle, or collarbone, connects the sternum (breastbone) to the shoulder and can be broken after a fall onto the shoulder directly or on an outstretched arm. Many fractures, particularly in non-athletes, are allowed to heal without surgery. Recently, however, orthopedic surgeons are choosing to treat these fractures surgically to ensure better anatomic healing and to shorten the time an athlete can be cleared to return to contact. Surgical repair of clavicle fractures once meant 6-12 weeks of rehabilitation, but players are now returning to play very quickly. While it shouldn't be considered the norm, Marques Colston returned to the field after clavicle surgery in less than three weeks in 2011.
Knee Injuries
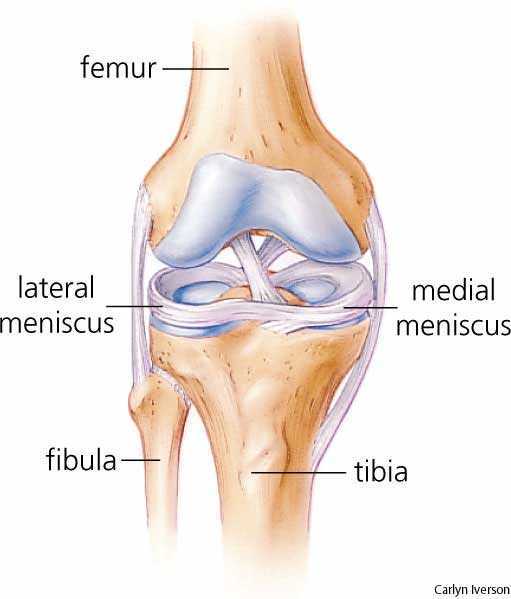
Anterior Cruciate Ligament (ACL) Sprain

The ACL is the critical knee ligament preventing the shin bone from sliding forward or rotating too far when the knee is under stress. ACL tears can occur after a direct blow to the knee or without contact when a player makes a sudden cut or pivot. The ACL also contains vital proprioception receptors that help a player "sense" where his knee is in space. Though a player's ACL may be functional intact and stable a few months after reconstruction, it can take as long as 18 months for a player to sense that his knee is stable under stress.
Though Grade 1 and 2 ACL strains can occur, direct blows and non-contact injuries to the ACL are most commonly complete tears requiring surgical reconstruction of the ligament. Surgery is usually delayed a few days to lessen the risk of scar tissue formation and sometimes longer to allow an accompanying MCL tear to heal and allow for more aggressive initial rehabilitation. Though it's possible to compete at a high level without an intact ACL (i.e. Hines Ward), it's rare to find a player with muscles strong enough around the knee joint to compensate and reconstruction is always recommended for an elite athlete after a complete tear.
Arthroscopic surgical techniques and accelerated rehabilitation schedules have shortened the time to return from ACL reconstruction to as short as six months. Associated injuries like MCL sprains and meniscal tears or the development of scar tissue in the knee joint necessitating an additional surgical procedure can lengthen recovery times to 9-12 months. It's again important to note that those timeframes correspond only to an intact and stable ACL that can be cleared for contact and that full recovery of proprioception may take longer.
Medial Collateral Ligament (MCL) Sprain
The MCL provides stability to the inside of the knee and is often injured when a player is hit on the outside of the knee, stretching the inside of the knee joint on the opposite side of the hit. Grade 1, 2, and 3 injuries are all commonly seen in football players. Many players, particularly offensive linemen, choose to wear braces to help prevent MCL injuries.
MCL injuries, including complete tears, are allowed to heal without surgery. Rarely, very severe Grade 3 injuries or symptoms of chronic instability necessitate surgical reconstruction. Recovery and return to play depends on the severity of strain. Players with Grade 1 strains may be able to play with a brace and not miss time. Most players with a Grade 3 MCL tear will miss six weeks while the ligament fully heals.
Meniscal/Articular Cartilage Tears
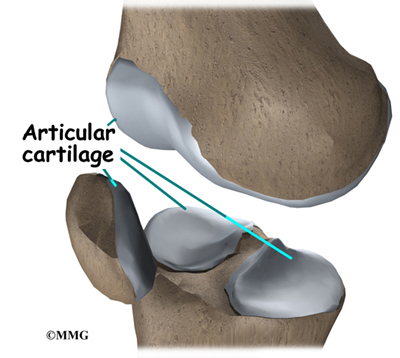
There are two kinds of cartilage in the knee joint. The surfaces of the femur, tibia and patella are covered with smooth, articular cartilage that allows the knee to slide easily during movement. The knee also has two semi-circular shaped cartilage-like structures, the medial meniscus (inside of knee) and lateral meniscus (outside of knee), on the surface of the tibia. These meniscal cartilages act as shock-absorbers and help prevent injury to the articular cartilage of the knee.
Both of these structures can be injured, usually when the knee is bent and then twisted. Both structures are also prone to degenerative changes, which can be accelerated by the high wear-and-tear football environment. Pain and swelling is common, with limited range of motion also a frequent symptom of these injuries. Because there are areas of both structures, particularly the articular cartilage surfaces, with relatively poor blood supply, no two injuries are alike and healing and recovery can be difficult to predict.
Meniscal tears can be repaired (usually when the injury is to the thicker part of the meniscus at the outside of the joint) or the torn fragment can be removed or trimmed. To prevent damage to the articular cartilage and its associated high risk of arthritis, standard of care is to repair or preserve as much of the meniscus as possible. Players who have meniscal fragments removed can return to play much more quickly (one to two weeks) than those who have their meniscus repaired (six weeks and often longer).
Articular cartilage wear and tear cannot be repaired surgically and the cartilage will not regenerate. Players with significant articular cartilage loss are often said to have a "bone-on-bone" condition. Often, microfracture surgery - a procedure in which multiple small holes are drilled into the bony surface to stimulate new (though not as durable as the original) cartilage growth - is the only option for symptom relief. The success of microfracture surgery is dependent on many factors and rest and rehab periods often extend past six weeks.
Patellar Tendon Tear
The patellar tendon runs from the patella (kneecap) to the upper surface of the tibia (shin) and is necessary to extend the leg at the knee joint. Ruptures usually occur after a period of chronic inflammation and irritation and happen when the knee is bent, the foot planted and the thigh muscles contract to prevent a fall or change direction (i.e. landing after a jump or trying to prevent tripping to the ground).
A torn patellar tendon in an elite athlete is always repaired surgically. Calcifications within the tendon, proximity of the tear to the kneecap and other associated injury can complicate repair. Rehabilitation and recovery lasts a minimum of six months and it may take 9-12 months before the large quadriceps muscles return to their former bulk and strength. Weakness, loss of explosiveness and reduced range of motion are common complications after a patellar tendon repair.
Recent advances in surgical techniques and the continuing trend of aggressive rehabilitation schedules are promising (as they've been for Achilles tendon repairs) but it's still too soon to assess how successful the changes in approach may be.
Foot and Ankle Injuries
Ankle Sprains
The classic (low or lateral) ankle sprain occurs when the foot is flexed inward (inversion injury). These common injuries are treated with boot immobilization and aggressive rehabilitation and rarely result in loss of playing time. Grade 3 injuries with chronic instability or avulsion fractures of the fibula may require surgical fixation and a much longer recovery time.

A high ankle sprain is an injury to the ligamentous structure (syndesmosis) that stabilizes the two bones of the lower leg. It commonly occurs when the foot is forcefully rotated outward away from the lower leg. High ankle sprains heal more slowly than low ankle sprains, with Grade 1 injuries usually requiring one to two weeks of rehabilitation and Grade 2 sprains often needing three to four weeks to heal. Slow healing injuries may take longer. Grade 3 high ankle sprains require surgical fixation of the ligament and are also usually associated with fractures to the fibula. There are reports of return to full activity following surgery in six weeks, with 8-10 weeks a more conservative and realistic estimate in most cases.
Achilles Tendon Rupture
The Achilles tendon is the largest tendon in the body and attaches the calf muscles to the back of the heel. A ruptured Achilles tendon most commonly occurs when a player's full body weight comes down on a straight leg with the ankle fully flexed. Unlike a patellar tendon tear, it is not uncommon for a healthy Achilles tendon to rupture under stress, but players with chronic irritation and calcification of the tendon are at higher risk of injury.
Surgical reconstruction is recommended for both significant partially torn and completely ruptured tendons. Minimally invasive surgical techniques and aggressive rehabilitation schedules to minimize loss of range of motion have shortened recovery times to six months in many cases. In recent years, many players have recovered to near their previous levels of activity and function, though loss of explosiveness remains a significant concern.
Lisfranc Dislocation / Fracture

The Lisfranc joint is a complex of many joints between the long bones of the foot and the smaller bones between the foot and ankle and includes the Lisfranc ligament, which connects the second metatarsal to one of the smaller bones in the middle of the foot. Injuries in this area include sprains to the ligament, fractures to the bones surrounding the joint and dislocations. The most common mechanism of injury is relatively low impact - another player falls on the back of the foot or heel while the foot is planted and flexed with the toes on the ground.
Minor ligament sprains can cause enough displacement in the joint complex to cause significant pain and instability in the middle of the foot. Low grade sprains with very little joint displacement can be treated without surgery, but require immobilization and crutches for at least six weeks. Joint displacements as little as 2 mm are considered to be Grade 3 sprains due to the high likelihood of instability to the joint. Those injuries and/or any associated fractures must be treated surgically.
The severity of the dislocation, location of any associated fractures, presence of articular cartilage damage and possibility of damage to blood supply to the region all affect the success of surgical repair. Outcomes have improved over time, but chronic pain and early arthritis in the joint remain common long term complications. Recovery and rehabilitation after surgery is usually expected to take six months, though some studies are considering whether removing surgical screws sooner may shorten recovery times.
Plantar Fasciitis

The plantar fascia is a tough ligament that supports the arch of the foot and runs from the base of the toes to the heel. Plantar fasciitis is usually an overuse syndrome, with repeated stress along the arch leading to a cycle of inflammation and loss of elasticity in the structure and degenerative changes. The plantar fascia can also rupture with continued stress to an already inflamed area.
Immobilization, orthotic shoe inserts, stretching and massage programs and steroid injections may help to limit the pain associated with plantar fasciitis, but prolonged rest and limiting the stress to the ligaments are necessary to resolve the symptoms. If those interventions aren't successful, surgery to release part of the plantar fascia may be recommended to relieve tension in the ligament. Chronic pain and gait changes remain possible after surgery.
Turf Toe
Turf toe is an injury to the ligamentous capsule that surrounds the joint between the base of the big toe and the long bone of the foot behind. These injuries most commonly occur when the foot is flexed and planted and the first toe is hyperextended, either when planting and changing direction or when another player lands on the foot from behind.

Because the small area assumes a load many times the weight of the body during football-related activities, even Grade 1 injuries can be difficult to recover from quickly. Taping to support the toe joint, steel insole plates, rest and immobilization are likely treatments, but significant Grade 1 and most Grade 2 injuries can take two to four weeks to fully heal. Grade 3 injuries may take 4-6 weeks. Since many players will attempt to play through or return quickly with a toe sprain, the time to full recovery and effectiveness is even longer.
If chronic pain or instability of the toe joint persists, surgery may be recommended. Recovery and rehabilitation usually lasts 3-4 months, though it may be at least six months before a player can return to his pre-injury level of function.
Fractured Bones
Broken bones are common and almost always require surgical fixation in football players. Long bone fractures in the arm and leg require often take four to eight weeks (and longer in some situations) to heal after surgery.
Broken hand, thumb and finger bones usually require pins or plate fixation, with return to play estimates dependent on the severity and location of the fracture, pain tolerance of the player and, oftentimes, the player's position. A lineman or linebacker may return to play sooner than a wide receiver or running back after a broken hand or finger due to splint sizes and the duties of their respective positions.
Rib fractures may take six weeks to heal. Flak jackets and pain management usually allow players to return to play quickly, but the number of rib fractures and fractures closer to the sternum usually necessitate longer recovery time.
Fractures to the fifth metatarsal (the bone along the outside of the foot), whether due to direct trauma or stress related, are often problematic due to poor blood supply to the area. Screw fixation is common, but fixation failures and chronic pain can occur and cause recurrent issues and missed playing time.
Concussion
A concussion is defined as any traumatic and temporary impairment of neurologic function. Though sometimes applied confusingly in the past, this definition includes all brain injuries regardless of severity or length of symptoms. Minor symptoms, including a player having his "bell rung" without loss of consciousness or memory loss or an injury associated with only a few minutes of headache or confusion, should correctly be considered a concussion. Concussions commonly occur after a direct blow to the head, but rotational impacts around the jaw and neck can also cause a concussion.
Athletes that have sustained one concussion are at increased risk of experiencing another and are especially vulnerable while the brain is recovering from a prior concussion. A second concussion before the previous concussion has fully resolved or more than three concussions often lead to more serious and prolonged symptoms. That vulnerability and the increased understanding of long-term effects like chronic traumatic encephalopathy have pushed the NFL toward a more rigorous evaluation and treatment plan for concussions on the sideline and between games.
Though there are no standard grading systems or algorithms universally agreed upon in the medical community, concussions may be loosely divided into three groups. Grade 1 concussions are not associated with loss of consciousness or symptoms that last longer than 15 minutes. Grade 2 concussions are not associated with loss of consciousness but symptoms that last longer than 15-30 minutes. Grade 3 concussions include injuries with loss of consciousness of any duration. There is a good argument that a large gray area exists between Grade 2 and 3 concussions using the above criteria, i.e. an injury without loss of consciousness but prolonged neurologic symptoms is just as concerning as an injury associated with a brief period of loss of consciousness and short period of neurologic symptoms.
The NFL uses its own algorithm to decide how quickly a player with a concussion may return to play. Any player with concussion-like symptoms must be immediately removed from the game and examined. That exam should include both physical and cognitive exams, which are then repeated after a period of observation. If a player who had only mild symptoms shows no symptoms after 15 minutes of observation and has no concerning exam findings, return to play that day is at the discretion of the medical staff. A player with more severe initial symptoms, whose symptoms do not clear after a period of observation or who had a recent concussion should not be allowed to return to play that day.
The algorithm also includes strict guidelines for clearing a player for future contact. A player must pass a series of neurologic exams, after 24-hour periods of no activity, light exercise, and more vigorous exercise. The process must be started over if there is any recurrence in symptoms. He must also pass cognitive tests (when compared to preseason healthy baselines) and be cleared by an independent neurologist. The process generally takes a minimum of four to five days.
The NFL continues to assess and incorporate measures to prevent concusssions. Education directed at the culture of underreporting head injuries by players and medical staff personnel, impartial sideline and press box observers, penalties and fines for helmet-to-helmet contact, mandatory use of mouth guards, improvements in helmet design and fit, and IMPACT testing are all intended to reduce the number of concussions and improve their management on the sideline.
Orthobiologic Treatments
Orthobiologics are a hot topic among orthopedic surgeons who treat professional athletes. Generated from natural substances in the body and often formulated into high concentration treatments, substances like platelet-rich plasma, bone marrow injections and other stem cell treatments and bone grafts may speed up the healing process and are becoming more frequently used therapies for many of the injuries discussed above.
Platelet Rich Plasma (PRP)
PRP injections have gained favor among NFL athletes in recent years looking for quicker healing of a variety of injuries. Platelets are cell fragments carried in the blood that help form clots, but also contain growth factors that promote healing of connective and vascular tissue. When a blood sample is spun and separated, a plasma concentrate that contains 90% platelets can be generated - platelet-rich plasma.
PRP injections remain controversial in the orthopedic community. They have been used for tendonitis and muscle strains and to assist in fracture healing and ligament repairs. Some studies report dramatic improvements and others no improvement at all. There is some concern that some growth factors may worsen outcomes by contributing to scar tissue, particularly when used to aid muscle healing. Expect to hear more players being treated with PRP, with much more research to standardize the amounts and types of growth factors included in each treatment and determine which injuries PRP is most successful on the horizon.
Bone Marrow Aspirate / Stem Cell Injections
Stem cells are immature cells with the potential to become many different types of cells based on where they are in the body and how they're influenced by their environment. When they arrive at an injury site naturally or are introduced in higher concentrations by injection, they can develop into new bone, muscle, ligament or cartilage cells.
Stem cells can be removed from a person's bone marrow (usually in the hip) or harvested by donation. The small amount of stem cells in the marrow sample must be separated, grown and expanded in the laboratory, a process which can take as long as three weeks, before they are injected at the injury site. Like PRP treatments, the use of bone marrow treatments (stem cell therapies and bone matrix) is a relatively new treatment, with more studies describing its effectiveness and success expected soon.
Pain Killing Injections
Pain killing injections are common in the NFL. A variety of medications are used in a variety of locations for many reasons. The three most common types of injections are anti-inflammatory (e.g. Toradol), anesthetic (e.g. Marcaine, etc.) and steroid (i.e. cortisone shot).
Game day Toradol injections are probably the most common pain killing injections given. Toradol is an anti-inflammtory similar to ibuprofen that can be injected to relieve pain from an existing injury or to (hopefully) limit the expected soreness after a game. It's not a narcotic medication and is not addictive. Toradol may not completely mask the pain of an existing injury, but it's dual pain-relief, anti-inflammatory effects are considered a lifeline to many players, Like other anti-inflammatories, it carries a risk of ulcers, GI bleeding and kidney damage.
Players also sometimes receive anesthetic (numbing) injections with Marcaine or another similar medication (lidocaine, bupivacaine, etc). These injections can be used as a nerve block on gameday to relieve pain for a few hours, usually around a joint (shoulder, toe, etc) or a larger area (plantar fascia, rib fracture). These injections mask most, if not all, pain by deadening the nerve fibers in the area.
Anesthetic medications are also commonly used in conjunction with steroids to treat pain and inflammation in a joint on non-game days. These injections are often very effective, but may carry a risk of long-term arthritic conditions and changes to the skin overlying the injection site and the number of injections considered safe for a single joint is limited.
Please ask questions or send comments to me by email at bramel@footballguys.com or on Twitter at @JeneBramel.
